Ticks aren’t a “deep bush only” problem anymore. They show up on suburban trail systems, cottage properties, hunting access routes, dog parks, and the edge habitat most Canadians walk through without thinking twice. The tricky part is that a tick bite is often painless, ticks can be very small (especially in earlier life stages), and people often don’t notice attachment until hours—or days—later.
That’s why the real risk isn’t “being outside.” The risk is failing to run a repeatable, low-stress protocol: avoid bites → check → remove correctly → document → monitor for symptoms.
This feature is written for Canadians who want clarity. Not panic. Not internet folklore. Not vague “be careful” advice. Just practical steps that match what Canadian public health guidance actually says.
Important note: This article is educational and does not replace medical advice. If you develop symptoms after a tick bite or you’re worried about your risk, contact a healthcare professional or your local public health unit.
What ticks can do in Canada: real risk (not fear)
Most tick bites do not lead to infection. But some ticks can carry pathogens that matter, and risk varies by region and exposure.
Lyme disease is the headline risk
Lyme disease is the most widely known tick-borne illness in Canada and can cause early symptoms like an expanding rash and flu-like illness; later symptoms can involve joints or neurologic problems if untreated. Public Health Agency of Canada
Canada’s Lyme disease information hub is here:
Public Health Agency of Canada
Ontario (and other provinces) also track additional tick-borne diseases
Ontario’s tick-borne diseases page provides provincial-level guidance and removal advice.
Ontario
Public Health Ontario’s Ontario Vector-Borne Disease Tool includes surveillance categories (e.g., Lyme disease and other vector-borne diseases) and established risk area information.
Public Health Ontario
Some Ontario public health units also reference tick-borne diseases of public health significance, including anaplasmosis, babesiosis, Lyme disease, and Powassan virus infection. NWHU+1
When ticks are active in Canada: “tick season” is longer than you think

Many Canadians treat ticks as a “summer-only” problem. But public health prevention guidance is built around conditions, not calendar dates. Practical risk rises when you’re in tick habitat and ticks are active (often in spring through fall, and sometimes beyond depending on conditions).
The Public Health Agency of Canada (PHAC) provides prevention guidance here:
Canada
PHAC’s Lyme disease prevention toolkit is here:
Canada
Practical field rule: If you’re in tall grass, brush, leaf litter, or trail edges, act like ticks are possible. It’s not paranoia—just routine.
Where ticks actually live: the “edge habitat” truth
Ticks don’t jump or fly. They typically “quest” on vegetation and latch onto animals (or you) when you brush past. That means the highest-risk areas are often the most ordinary:
- trail edges where shrubs touch your clothing
- long grass beside paths
- leaf litter under trees
- bushy transitions between lawn and forest
- wildlife corridors (deer trails, game paths)
PHAC’s prevention toolkits consistently emphasize clothing barriers, repellents, staying on paths, and post-outdoor checks—because those are the practical points where exposure happens. Canada+1
PHAC “Check Prevent Take Action” PDF (simple checklist):
Government of Canada Publications
Real Prevention: what actually works (layered, repeatable, not extreme)
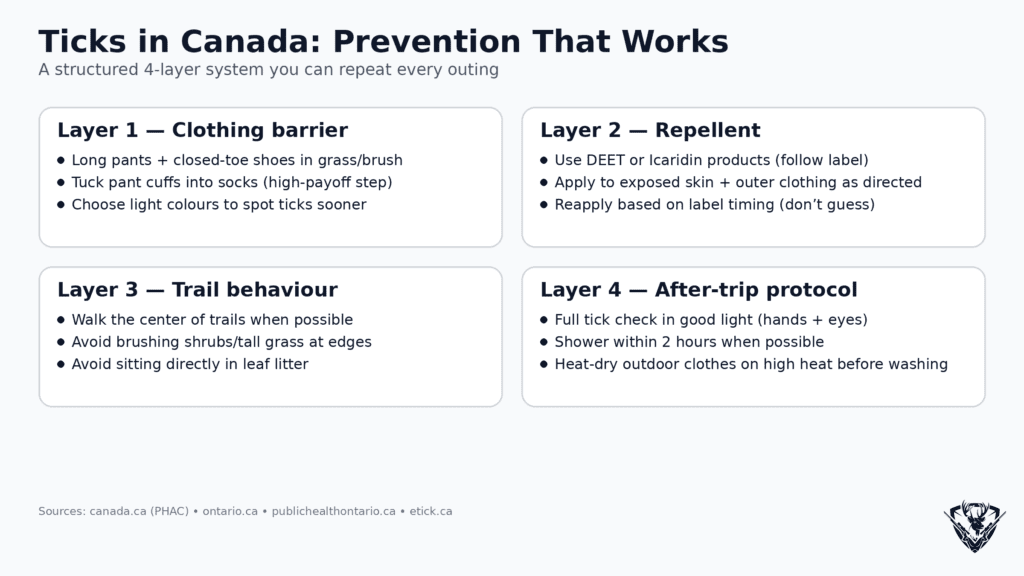
If you want prevention that works in the real world, think layers:
- Clothing barriers
- Repellent (correct ingredients, used correctly)
- Trail behavior
- After-trip protocol (check + shower + laundry heat)
Layer 1: Clothing barriers (boring, but high payoff)
PHAC recommends protective clothing measures such as long sleeves and pants, and tucking pants into socks. Canada+1
- wear closed-toe shoes
- wear long pants
- tuck pants into socks (one of the highest payoff steps)
- wear light-coloured clothing to spot ticks more easily Canada+1
PHAC prevention page: Canada
Lyme disease prevention toolkit: Canada
Layer 2: Repellent (DEET or icaridin) + permethrin-treated clothing
PHAC’s prevention guidance includes repellents containing DEET or Icaridin and also references permethrin-treated clothing (follow label directions). Canada+1
PHAC prevention page: Canada
PHAC prevention toolkit: Canada
Important: Always follow label directions—especially for kids.
Layer 3: Trail behavior (free prevention that actually matters)
PHAC’s prevention materials emphasize staying on paths and avoiding brushing against vegetation. Government of Canada Publications+1
PHAC checklist PDF:
Government of Canada Publications
Simple habits:
- walk in the center of the trail
- don’t cut corners through brush
- avoid sitting directly in leaf litter
- if you do bushwhack, treat it like higher risk and do stronger post-trip checks
Layer 4: The after-trip protocol that prevents most problems
PHAC recommends showering/bathing within two hours to wash away loose ticks and doing full-body tick checks. Canada+1
PHAC prevention toolkit: Canada
PHAC checklist PDF (includes shower within two hours and dryer heat):
Government of Canada Publications
Heat matters: PHAC’s checklist also mentions putting clothes in a dryer on high heat for at least 10 minutes. Government of Canada Publications
Tick checks: how to do them properly (and fast)
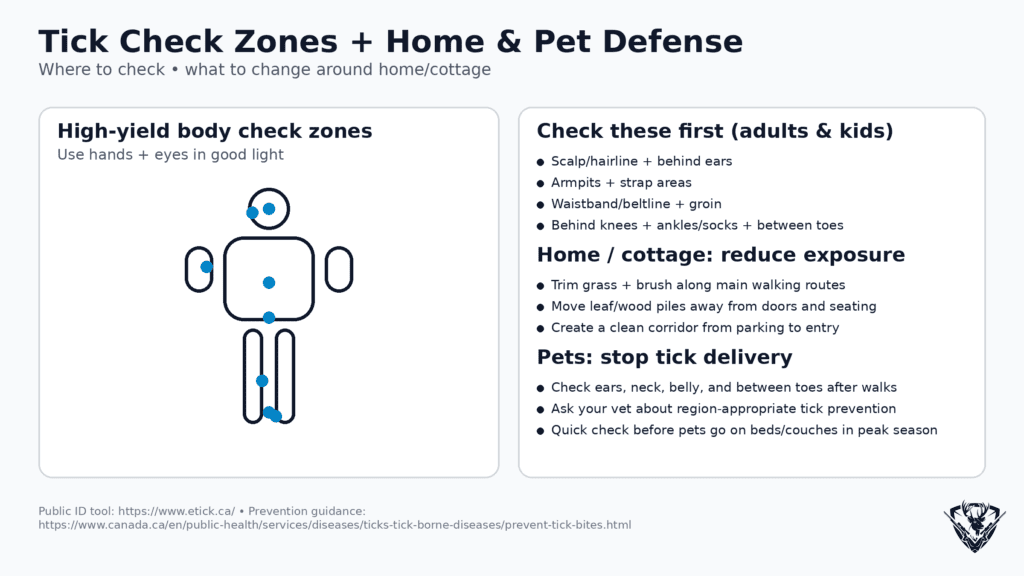
A tick check is not a glance in the mirror. It’s a systematic routine in good light.
High-yield check zones (adults)
- scalp and hairline
- behind ears
- armpits
- waistband / beltline
- groin area
- behind knees
- ankles and socks
- between toes
Kids: where ticks get missed most
- hairline/behind ears
- neckline
- waistband
- behind knees
Pro tip: Use your hands as much as your eyes. Small ticks can be easier to feel than see.
Pets: the “tick delivery system”
Pets can bring ticks into the home even if you did everything right on the trail.
- check around ears, neck, collar line
- under legs and belly
- between toes
- around tail base
If your dog sleeps on beds or couches, checks matter even more.
Real Removal: what to do the moment you find an attached tick
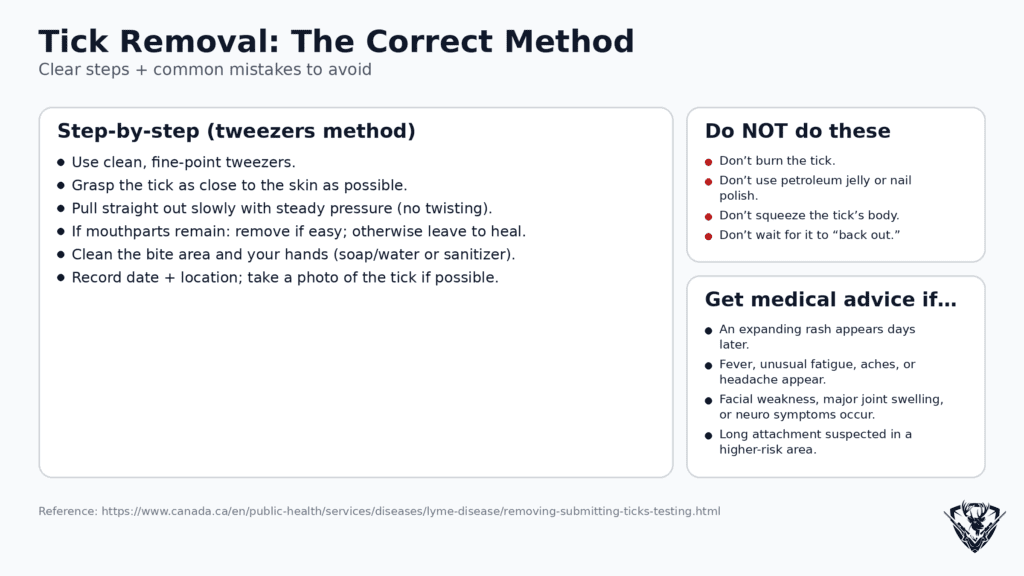
This is where people get misled by viral “life hacks.” Don’t improvise.
PHAC’s tick removal instructions: Canada
Step-by-step tick removal (PHAC method)
- Use clean, fine-point tweezers
- Grasp the tick as close to the skin as possible (near the head/mouthparts)
- Pull straight out, slowly and steadily
- Try not to twist or squeeze
- If mouthparts remain: remove them with tweezers if easy; if not, leave and let skin heal
- Wash the area with soap and water or sanitizer Canada+1
Ontario’s tick-borne diseases page also emphasizes fine-tipped tweezers and not using matches, nail polish, etc.:
Ontario
Many local Ontario public health units reinforce these “don’ts” as well (example: Thunder Bay District Health Unit):
Thunder Bay District Health Unit
What NOT to do
Avoid:
- burning the tick
- petroleum jelly
- nail polish
- “suffocating” tricks
- twisting hard
These don’t improve outcomes and can delay removal. PHAC emphasizes prompt removal with tweezers. Canada+1
After a tick bite: the calm, specific decision path
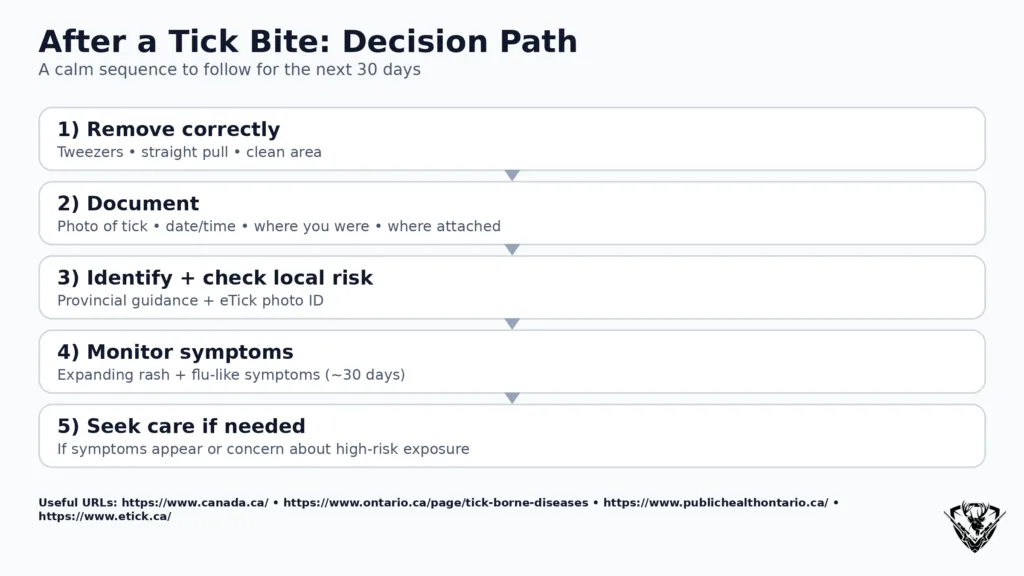
Here’s the balanced approach that prevents both underreacting and spiraling.
Step 1: Remove it correctly
PHAC removal page: Canada
Step 2: Clean the area
Soap/water or sanitizer (PHAC guidance). Canada
Step 3: Document the bite (this is the authority move)
Record:
- date/time removed
- where you were (park/trail/region)
- where on the body it was attached
- take a photo of the tick (if possible)
Step 4: Monitor for symptoms for ~30 days
Ontario clinical guidance frames symptom monitoring after tick exposure and discusses early symptom timing. Health Quality Ontario
Ontario clinical guidance PDF:
Health Quality Ontario
Step 5: Know what symptoms should trigger medical advice
Lyme disease information hub (Canada):
Public Health Agency of Canada
If symptoms develop, especially:
- an expanding rash (often >5 cm)
- fever, chills, fatigue
- headache, muscle/joint pains
- neurologic symptoms
seek medical advice.
Local public health algorithms also note that small rashes that appear quickly may be hypersensitivity/irritation rather than Lyme—timing and size matter (example: Ottawa Public Health clinician algorithm). Ottawa Public Health
Ottawa algorithm PDF: Ottawa Public Health
Tick identification and “testing”: what Canadians should actually do
People often ask: “Should I get the tick tested?”
In Ontario, there are two different concepts:
- Identification (What tick is it?)
- Testing (Does it carry something?) — which is not a simple consumer workflow.
Public Health Ontario’s Tick Submission and Testing FAQ:
Public Health Ontario
That FAQ includes practical details such as turnaround times and process notes. Public Health Ontario
A practical public option: photo-based identification (eTick)
eTick is a public platform for image-based identification and population monitoring of ticks in Canada. eTick
eTick site: eTick
eTick photo guide: eTick
Best practice: take clear photos and keep a simple log.
Antibiotics after a tick bite in Ontario: when prophylaxis is considered
This is where online advice is most misleading. Preventive antibiotics are not “for every tick bite.” Ontario has specific criteria frameworks.
Public Health Ontario antibiotic prophylaxis algorithm (PDF):
Public Health Ontario
That algorithm describes high-risk criteria that must be met (including time sensitivity such as tick removal within 72 hours and other risk criteria). Public Health Ontario
Ontario clinical guidance (PDF): Health Quality Ontario
Key point: prophylaxis decisions should be made with a clinician and depend on your situation.
Property prevention: reduce tick habitat without turning your place into gravel
You don’t need to sterilize a yard. You need to manage the edges where people and ticks interact.
High-yield actions:
- keep grass trimmed along walking routes
- reduce brush near doors and paths
- move woodpiles away from high traffic corridors
- avoid leaf litter piles near seating areas
- create a clean corridor from driveway to entry
PHAC prevention resources emphasize prevention actions and post-activity routines; the property approach is an extension of that logic. Canada+1
Top 10 Questions Canadians Ask About Ticks (Detailed Answers)
1) “How do I know if it was a blacklegged tick?”
What matters: tick species and your exposure region.
Practical approach:
- Take a clear photo of the tick (top + side)
- Use an identification platform like eTick (photo-based identification tool in Canada) eTick
eTick: eTick
Photo guide: eTick
If you’re in Ontario and you want to understand provincial tick disease context: Ontario
And for surveillance-style info (risk areas, trends): Public Health Ontario
Bottom line: Don’t rely on memory. Photo + ID beats guessing.
2) “How long does a tick need to be attached to be a problem?”
Risk generally increases with longer attachment, but the correct move is always:
- remove the tick correctly as soon as you find it Canada
- document
- monitor symptoms
Ontario resources discuss attachment/time windows in prophylaxis algorithms and clinical guidance. Public Health Ontario+1
PHO prophylaxis algorithm (PDF): Public Health Ontario
Ontario clinical guidance (PDF): Health Quality Ontario
Practical reality: most people can’t precisely know attachment time. That’s why documentation + symptom monitoring is important.
3) “What if the head breaks off?”
PHAC addresses this directly:
- remove remaining mouthparts with tweezers if you can
- if you can’t easily remove them, leave them and let skin heal Canada+1
PHAC tick removal page: Canada
Why not to panic: retained mouthparts can cause local irritation, but it’s not the same thing as “the tick is still attached and feeding.”
4) “What’s the correct way to remove a tick—step by step?”
PHAC’s step-by-step is the gold standard:
- fine-point tweezers
- grasp close to skin
- pull straight out slowly
- don’t twist
- clean afterwards Canada+1
PHAC page: Canada
Ontario page: Ontario
Local reinforcement example: Thunder Bay District Health Unit
5) “Should I use alcohol, Vaseline, or burn it off?”
No. PHAC and Ontario guidance emphasize tweezers and prompt removal, not gimmicks. Canada+1
PHAC removal: Canada
Ontario: Ontario
6) “What does an early Lyme rash actually look like?”
The “bull’s-eye” stereotype can be misleading. Some clinical/public health resources describe erythema migrans (expanding, typically >5 cm) and note variability.
Canada Lyme disease info: Public Health Agency of Canada
Ottawa clinician algorithm notes rash size/timing and that quick, small rashes may be hypersensitivity. Ottawa Public Health
Practical approach: Don’t self-diagnose by Google images. If you’re unsure, document with a photo and consult a healthcare professional.
7) “Can I get preventive antibiotics after a tick bite in Ontario?”
Sometimes, in certain higher-risk situations—Ontario has an algorithm for this that emphasizes time windows and risk criteria. Public Health Ontario+1
PHO algorithm (PDF): Public Health Ontario
Ontario clinical guidance (PDF): Health Quality Ontario
Key point: This should be decided with a clinician because contraindications and risk criteria matter.
8) “What’s the best repellent in Canada for ticks?”
Canadian public health guidance commonly points to repellents containing DEET or Icaridin and following label directions. Canada+1
PHAC prevention page: Canada
PHAC prevention toolkit: Canada
Practical approach: Choose one that fits your family situation and use it correctly—application and reapplication matter.
9) “Do I really need to shower after being outside?”
PHAC’s prevention guidance includes showering or bathing within two hours to wash away loose ticks. Canada+1
Checklist PDF: Government of Canada Publications
Why it helps: It removes unattached ticks and forces you to do a quick body scan.
10) “How do I reduce ticks around my cottage or property?”
Focus on where people and pets actually move:
- trim brush and tall grass along paths
- move leaf litter piles away from seating zones
- keep woodpiles away from high-traffic corridors
- make a clean corridor from parking to door
- tick-check pets after they roam
Use the same prevention principles PHAC emphasizes—reduce contact with tick habitat and apply consistent checks. Canada+1
The short, calm summary you can trust
- Real prevention works when it’s layered: clothing + repellent + trail behavior + post-trip check/shower/dryer heat. Canada+2Canada+2
- Real removal is fine-point tweezers, straight pull, clean afterward. Canada+1
- Real follow-up is documentation + symptom monitoring + medical advice if symptoms develop. Health Quality Ontario+1